6 Questions to Ask When Evaluating a Cleft-Affected Child

Are you evaluating or seeing a child with a history of a cleft palate? Here are six questions to ask or keep in mind!
When seeing a cleft-affected child, it’s important to remember that their anatomy is different, which can impact their speech, language, and resonance. Because of this, treatment may differ from a non-cleft-affected child.
What prior surgeries has the patient had? Are there any upcoming surgeries with their team in the coming months?
Has the patient’s hearing been checked recently? Is their ENT continuing to follow up with the patient if ear tubes were placed?
Children with cleft palate are more likely to get fluid in the middle ear and ear infections. This can cause mild to moderate hearing loss. This can affect speech and language development since the child may not fully and accurately hear speech sounds and words.
Eustachian tube dysfunction is common and present in over 90% of infants with cleft palates and leads to middle ear changes responsible for permanent hearing loss in adulthood. Some syndromes related to cleft palates have hearing loss associated with them, such as Stickler syndrome. Hearing loss is present in more than 50% of the adult cleft palate population. Those who are hard of hearing have a tendency to remain more hypernasal.
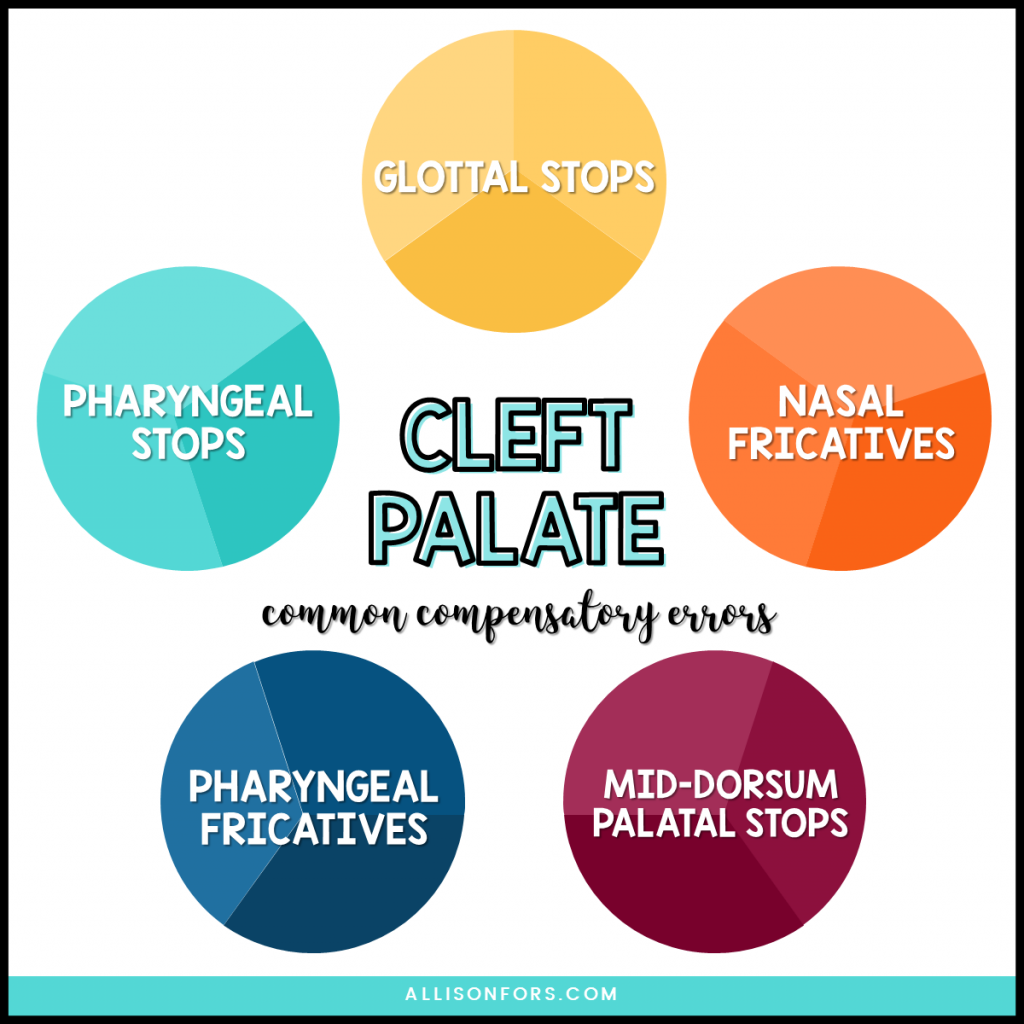
Do I hear any compensatory errors, such as glottal stops, pharyngeal stops, nasal fricatives, or pharyngeal fricatives?
Compensatory errors are abnormal articulation placement due to abnormal structure. These are most often errors of placement, not voice or manner. These errors may persist after palate repair due to learned behavior and require speech therapy to remediate. Read more about compensatory errors.
Do I hear any hypernasal speech or hyponasal speech?
Hypernasal speech is when there is too much nasal resonance and airflow though the nose, especially on vowels and voiced consonants. Hypernasality does not affect voiceless consonants, and it is most associated with velopharyngeal dysfunction.
Hyponasal speech is when there is too little nasal resonance and airflow through the nose, primarily on nasal consonants (m, n, ng.) This can be due to allergies, enlarged adenoids, upper respiratory infections or sinus infections.
Do I hear any obligatory nasal air emissions?
Nasal air emissions are the audible release of bursts of air through the nose during speech. It only occurs on consonants, particularly pressure consonants and voiceless sounds (p, b, t, d, k, g, s, z, ch, sh, j, etc.) It affects articulation – not resonance. Consonants become weak or omitted. The child may use abnormal speech sounds (such as a hard “uh” instead of /g/) due to the lack of oral air pressure.
They may occur due to velopharyngeal insufficiency or a fistula. Although, larger velopharyngeal openings may be inaudible.
You can hold a mirror under the nose and look for fogging during voiceless oral pressure consonants; or hold one end of a straw by the nose while the other end is at your ear to listen for airflow during the production.
Are these speech and resonance errors compensatory or obligatory? Will therapy alone fix these issues, or should I refer to a craniofacial team for further information?
SLPs may refer to an ENT specialist when they suspect that the patient’s speech or language is caused by a structural problem or medical condition in the ear, nose, or throat. Speech therapy cannot fix hypernasility, hyponasailty, or nasal air emission that is from velopharyngeal dysfunction. Read more about when to refer to ENTs.

What else would you add while evaluating a cleft-affected child for speech-language intervention?
You may also be interested in reading:
Cleft Lip and Palate Topic Page