Cleft Lip & Palate
This page is a compilation of information related to speech intervention in those with cleft lip and/or palate. Discover research, ideas, websites, and resources! Bookmark this page or save it to Pinterest with the image at the bottom.
Cleft lip and palate can co-occur or be independent of one another. A child may also have a submucous cleft, which is oftentimes difficult to detect because the mucous membrane covers the cleft. It is common for children born with a cleft lip and/or palate to need speech intervention at some point. Over half of these children will need speech therapy; however, most will develop normal speech by age five.
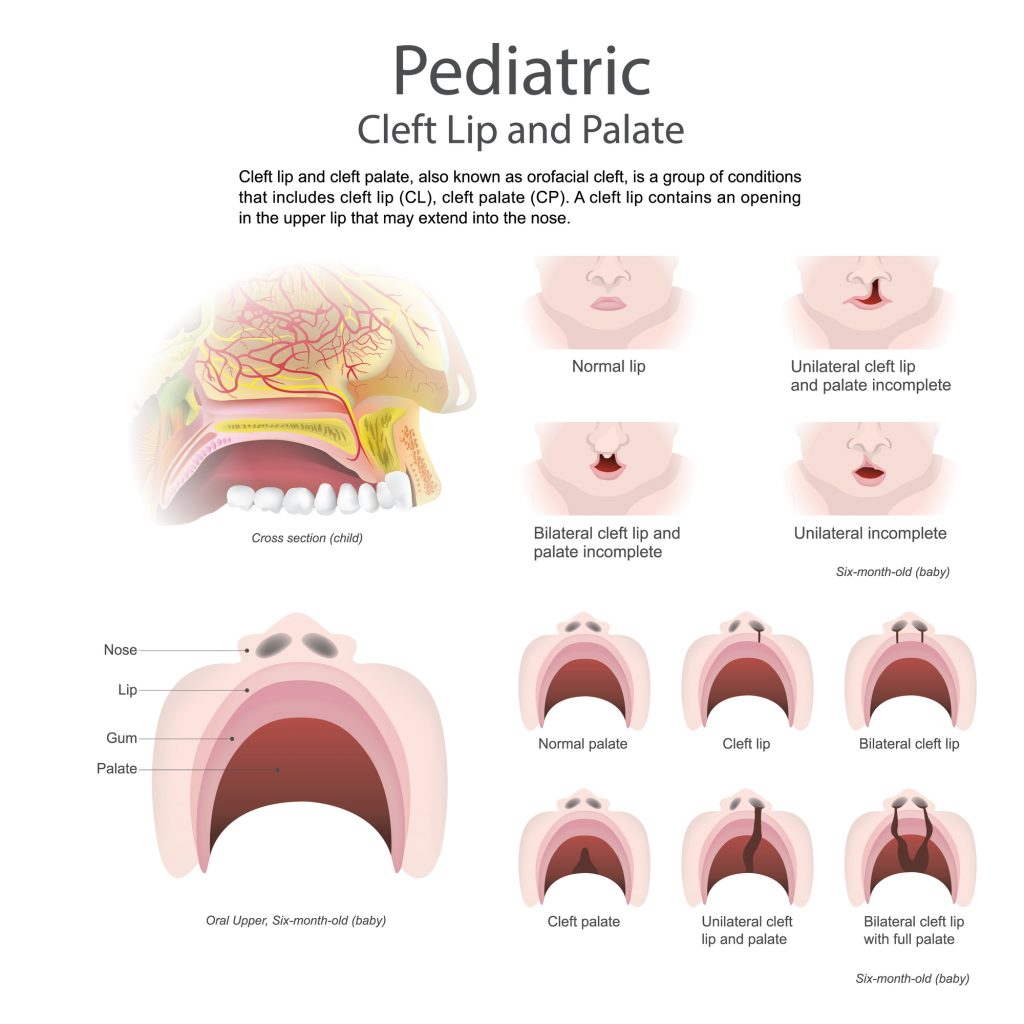
CLEFT LIP AND PALATE REPAIRS
Cleft lip repair typically occurs between 3-6 months old and cleft palate repair typically occurs between 8-14 months old.
More surgeries may be needed as a child grows older, such as a pharyngoplasty.
Before palate repair: Babies with cleft palate produce vocalizations as much as babies who are not cleft affected, although they have delayed onset of babbling and first words and they acquire words more slowly. They also prefer words beginning with sonorants (vowels, nasals, liquids, and glides.) This is because these are the sounds they can make without a palate! Encourage /m,n,l,w,j/, “ng”, and vowels, as well as any tongue and lip movement. Some words to model are “me”, “more”, “no”, “mama”, and “wawa” for water, and other approximations. It is important to note that cleft babies are not affected receptively (unless hearing is impacted.) If they are not repeating words back, they are still learning and expanding their vocabulary.
After palate repair: Encourage the use of more sounds /p,b,t,d,k,g,s,z,f/ and target a greater variety of CV, CVC, and CVCV words.
FIRST SPEECH THERAPY SESSION
Gather a case history:
- family history of clefts and speech disorders
- birth history
- developmental milestones history
- medical diagnosis
- feeding history
- hearing/ear infection and vision history
- surgical history
- speech and language therapy history
Gather concerns:
- feeding
- breathing and snoring
- hearing loss
- psychosocial concerns
- speech intelligibility (for familiar adults and unfamiliar adults)
- resonance
Conduct an oral mechanism exam:
- visually examine the structure of the face, nose, eyes, ears, skull for proportion and symmetry
- lip closure and movement
- tongue elevation and movement
- look for tongue abnormalities, such as asymmetry, macroglossia, akyloglossia
- presence and size of the tonsils – large tonsils may affect resonance and airway
- look for any teeth malocclusions
- check for movement of the palate
- listen for resonance
Use phonemically loaded sentences for an informal assessment of overall intelligibility and to access other factors, such as hypernasality and other resonance disorders.
A Guide for Cleft Palate Speech Sampling
You can even get in contact with the craniofacial team’s SLP regarding the child. (Most children are followed by a craniofacial team starting at birth. This includes an SLP, audiologist, dietician, surgeon, dentist, orthodontist, social worker, nurse, and perhaps other professionals.)
SUBMUCOUS CLEFT SIGNS AND SYMPTOMS
A submucous cleft palate is an opening in the muscles of the soft palate, beneath the mucous membrane. These are things to look for in an oral exam, to listen for, and get a history on!
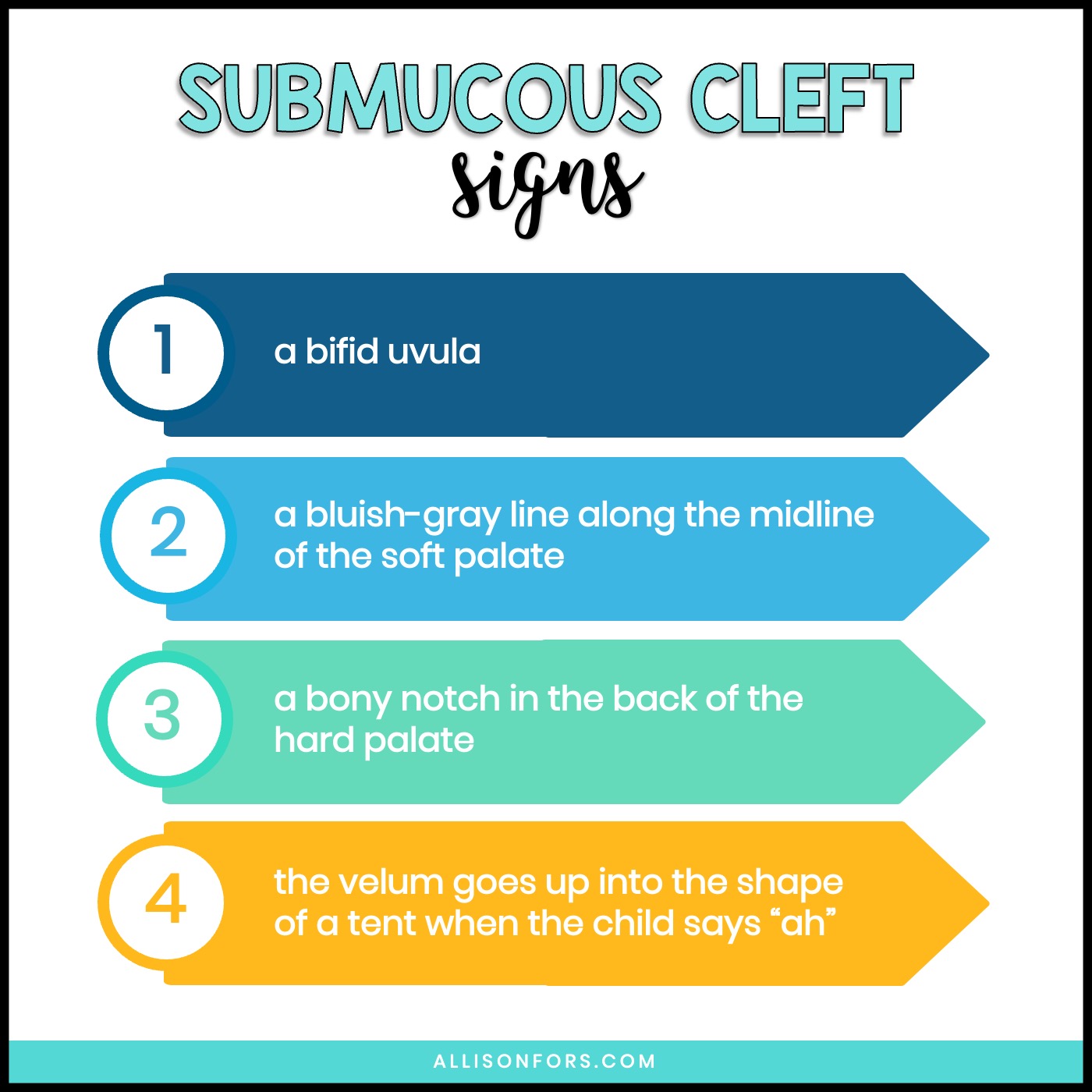
Potential signs:
1. a bifid uvula
2. a bluish-gray line tissue along the midline of the soft palate (this indicates the soft palate muscles are separated)
3. a bony notch in the back of the hard palate
4. the velum goes up into the shape of a tent when the child says “ah”
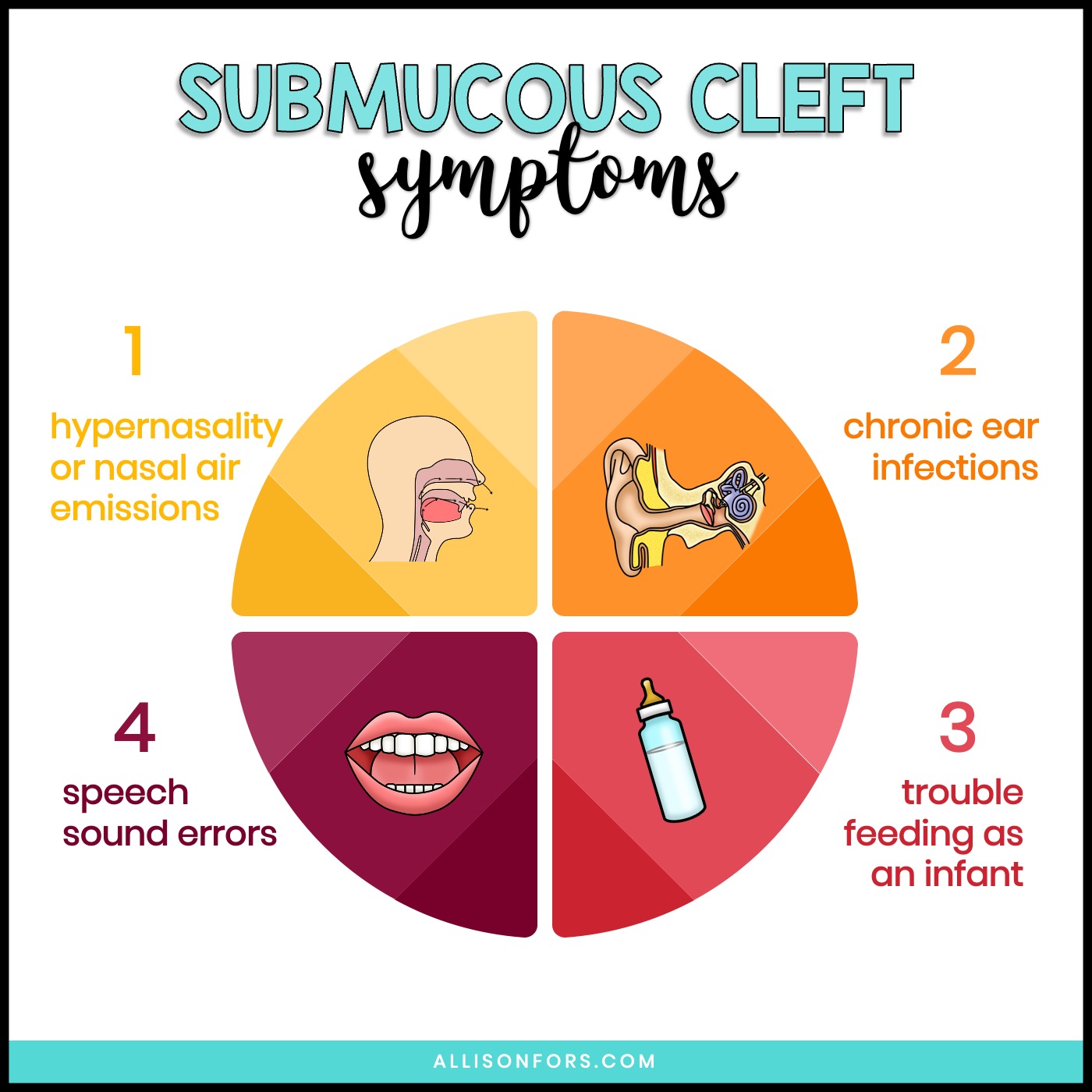
Potential symptoms:
1. hypernasality (“nasally sounding” speech) or nasal air emissions (hearing air leak out the nose during speech)
2. chronic ear infections
3. trouble feeding as an infant (taking a long time to feed, liquid coming through the nose, etc.)
4. speech sound errors
COMMON INTERVENTIONS NEEDED WITH CLEFT LIP AND PALATE
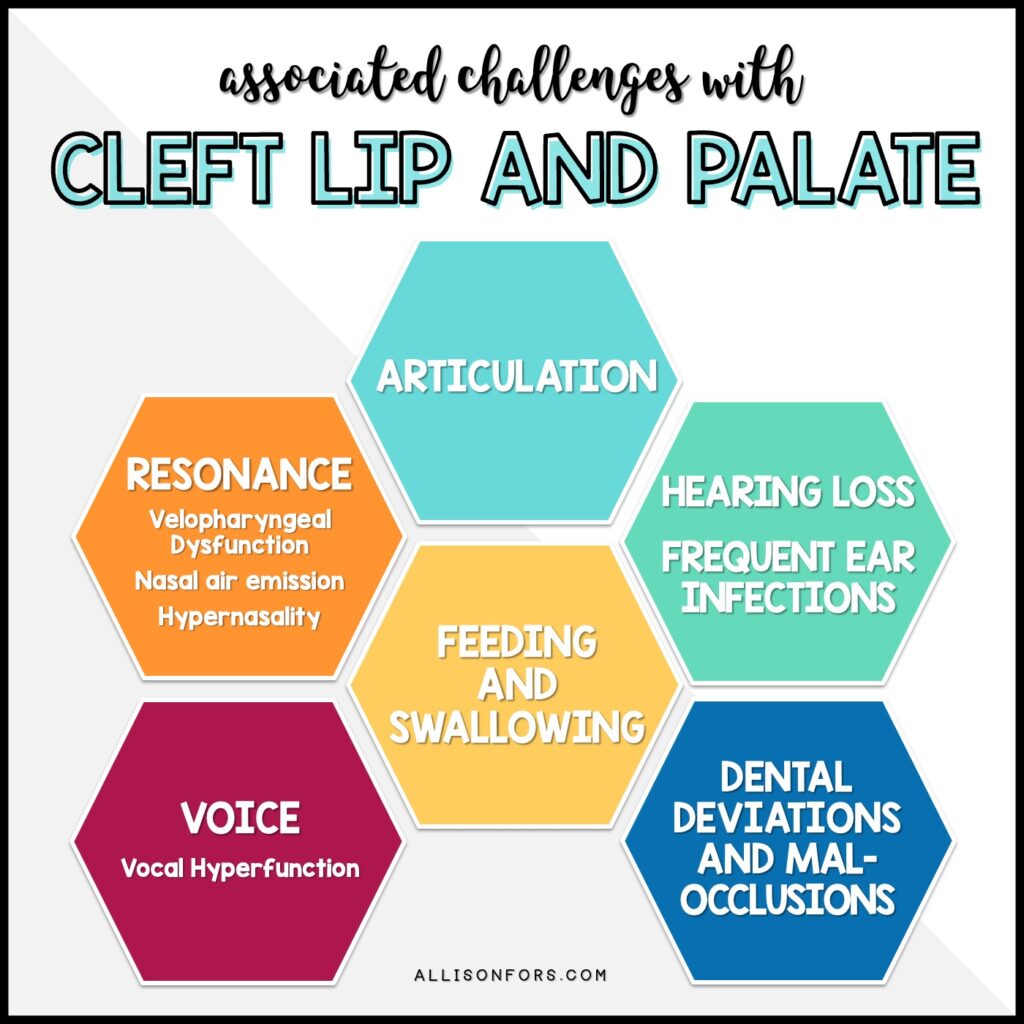
ARTICULATION: A child with a cleft lip may have typical articulation. Those with cleft palates or submucous palates are much more likely to need articulation intervention. Common speech sound errors include glottal stops, nasal fricatives, pharyngeal fricatives, and mid-dorsum palatal stops. Oral movement may be affected, such as reduced lip rounding or tongue elevation. Be sure to differentiate between the speech sound errors: obligatory, compensatory, or developmental.
VELOPHARYNGEAL DYSFUNCTION (VPD): A generic term for resonance disorders. VPD occurs when the velopharyngeal port does not have proper closure during speech or swallowing. Air leaks into the nasal passage due to the soft palate’s inadequate speed or range of function. This can result in nasal air emission, hypernasality, abnormal speech, and decreased intelligibility. All children with a cleft palate will demonstrate VPD prior to cleft repair.
NASAL AIR EMISSION: The audible release of bursts of air through the nose during speech.
HYPERNASALITY: A condition when air flows through the nasal passage during voiced consonants and vowels, causing too much nasal resonance.
VOCAL HYPERFUNCTION: A chronic condition when the glottis is overworked resulting in a strained voice, fatigue, or pain.
FEEDING AND SWALLOWING: Children with an isolated cleft lip can use a typical bottle or may be able to breastfeed. Children with a cleft palate oftentimes cannot breastfeed and use a specialty feeder, such as the Dr. Browns Specialty Feeder or Haberman bottle. These bottles don’t require the baby to produce suction and you can pace a baby with the Haberman bottle.
HEARING LOSS: Children with cleft palate are more likely to get fluid in the middle ear and ear infections. This can cause mild to moderate hearing loss. Eustachian tube dysfunction is common and present in over 90% of infants with cleft palates and leads to middle ear changes responsible for permanent hearing loss in adulthood. Some syndromes related to cleft palates have hearing loss associated with them, such as Stickler syndrome. Hearing loss is present in more than 50% of the adult cleft palate population. Those hard of hearing have a tendency to remain more hypernasal.
DENTAL DEVIATION AND MALOCCLUSIONS: Children with a cleft palate or lip are more likely to have dental abnormalities. This may include an overbite, underbite, crossbite, extra teeth, missing teeth, and teeth out of alignment. If the alveolar ridge is affected by a cleft, the teeth may be displaced or rotated. These dental differences may affect speech production.
Speech therapy cannot fix hypernasility, hyponasailty, or nasal air emission that is from VPD. Speech therapy is effective in teaching abnormal speech sounds placement caused by VPD. Refer to the craniofacial team!

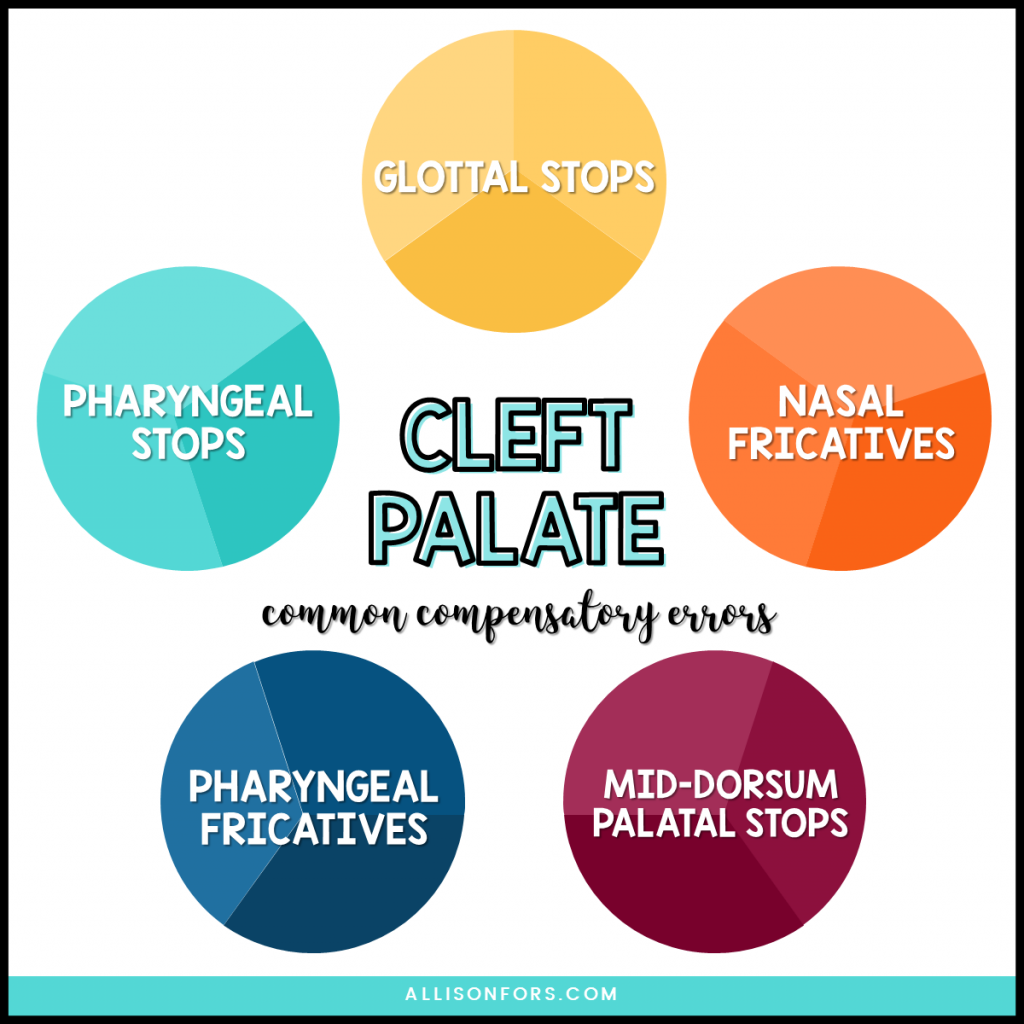
COMMON COMPENSATORY ARTICULATION ERRORS
Children with a cleft palate may learn to use abnormal speech sounds due to abnormal anatomical structures. These speech sounds are called compensatory errors and oftentimes persist after surgery due to learned behavior and require speech therapy to remediate. As SLPs and SLPAs, it is important to recognize and identify specific compensatory errors when working with this population. Approximately 25% of children with cleft palates use compensatory articulation errors and glottal stops are the predominant error!
GLOTTAL STOPS: A sound produced by bringing the vocal cords together and then releasing them suddenly instead of the tongue or lips. You may hear or use a glottal stop while producing certain words, such as “button”, instead of fully articulating the “t” in the middle of the word or in “uh oh.” A glottal stop is typically used for /p, b, t, d, k, g/ sounds. For example, a child with a cleft palate may say the word puppy as “uh-ih”.
NASAL FRICATIVES: When air is directed into the nasal cavity while producing a fricative sound such as /f, s, v, z/, “th”, and “sh”.
PHARYNGEAL FRICATIVES: When the wall of the throat is used to produce a fricative sound instead of with the tongue. This is typically used to substitute the /s, z/ and “sh” sounds.
PHARYNGEAL STOPS: When the back of the tongue contacts the wall of the throat to stop airflow. This is typically used to substitute the /k, g/ sounds but may be used for other oral stops or oral pressure consonants.
MID-DORSUM PALATAL STOPS: When airflow is stopped by the tongue contacting the middle of the roof of the mouth and used as a substitute for /t, d, k, g/. This error sounds like a production between a “k” and “t”.
Read more: Common Compensatory Errors
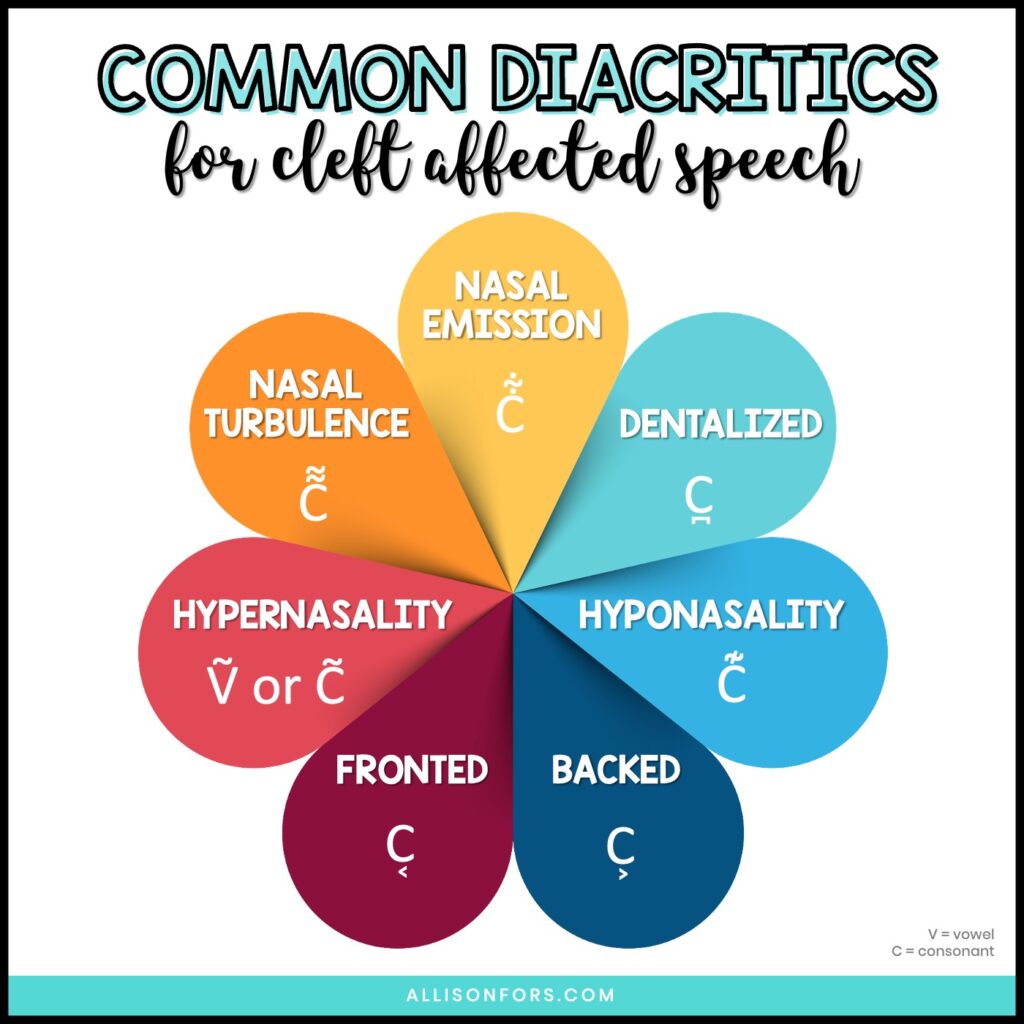
COMMON DIACRITICS
CLEFT LIP AND PALATE WEBSITES
Pam Marshalla – Cleft Palate and Resonance
ASHA Clinical Topics: Cleft Lip and Palate
ASHA Clinical Topics: Resonance Disorders
ASHA Evidence Maps: Cleft Lip and Palate Research Articles
ASHA Leader: 10 Common Questions About Cleft/Craniofacial Management Answered
ASHA Leader: Opening the Toolbox for Cleft Palate – Related Speech Disorders
American Cleft Palate-Craniofacial Association
CLAPA – Cleft Lip and Palate Association
RESEARCH ARTICLES
Speech Evaluation and Treatment for Patients With Cleft Palate
PROFESSIONAL DEVELOPMENT
Beyond Cleft Palate: Differential Diagnosis and Treatment of Velopharyngeal Dysfunction
English Cleft Palate Speech Therapy: Evaluation and Treatment
BOOKS
The Clinician’s Guide to Treating Cleft Palate Speech by Peterson-Falzone, Trost-Cardamone, Karnell, and Hardin-Jones (2nd ed.)
BLOG POSTS
Treating Cleft Palate: Q&A with a Craniofacial SLP
Common Cleft Palate Compensatory Errors
Sound Loaded Books for High Pressure Sounds
Signs and Symptoms of Submucous Cleft Palate
How to Help Speech Development Before Palate Repair
Questions to Ask When Evaluating a Cleft-Affected Child
Children’s Books About Cleft Lip and Palate
PODCASTS
Listen to a podcast episode where we discuss cleft speech and my personal experiences with a cleft-affected child:
De Facto Leaders – Cleft Palate, Resonance Disorders, and Market Research
SLPs Wine and Cheese – Velopharyngeal Insufficiency
Speechy Things – Hello from the Other Side: Becoming a NICU Mom
The Unexpected Podcast – Cleft Palate