
Treating Cleft Palate in Speech Therapy: Q & A with a Craniofacial SLP

Welcome and thanks to my guest blogger, Meg Lico, a Craniofacial SLP in New York!
Like many of you reading this blog, I have always loved being a Speech-Language Pathologist. During my graduate studies, I was lucky enough to have an amazing mentor with significant knowledge in the assessment and treatment of children with cleft lip and palate, and that is when I fell in love with this part of our field.
I have partnered up with Allison to help shed some light on what I do, how I treat, and how you can be more involved with the little ones on your caseload who may have a cleft palate or a craniofacial condition!
Many graduate programs do not have a cleft palate/craniofacial course, or, it is elective, so you are not alone in feeling apprehensive when a child with a complex craniofacial condition shows up on your caseload. This is often something I hear from school, private, and EI-based SLPs, who have amazing expertise in CAS, phonological disorders, autism, and so forth, but only see a couple of children on their caseload with cleft palate and craniofacial conditions every year. And that is OKAY!

The key here is to 1) soak up all of the continuing education and resources provided here and 2) coordinate with the patient’s cleft palate/craniofacial team Speech-Language Pathologist; not only can they give you insight into his current surgical timeline, orthodontic plan, and overall functioning, but he/she can also give you tips and tricks for evaluation in therapy.
I have multiple phone calls a week with school and EI-based SLPs about mutual patients (with consent from parents, of course), and we love learning from each other! I find that as much as they learn from me about this topic, I continue to learn so much from them about a number of different topics as well (and can I just say, school and EI SLPs are so creative!).
What does your usual day look like?
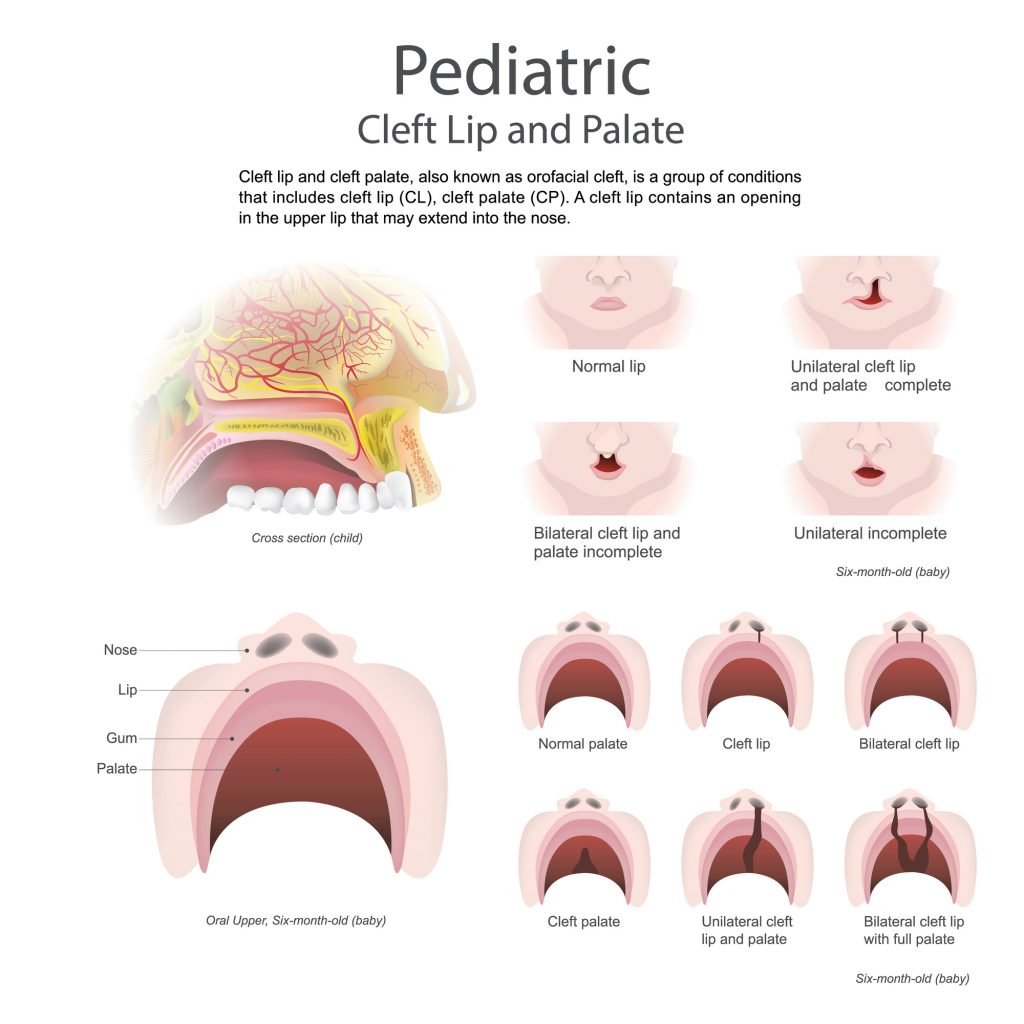
I assess and treat pediatric patients (and sometimes adults as well!) alongside our team members: plastic surgeons, orthodontists, social workers, psychologists, dieticians, care coordinators, and lovely nurse practitioners. We also work extremely closely with the otolaryngology team, audiology, and genetics. Together, we create an appropriate treatment plan for each child. We treat a number of different conditions: cleft lip +/- palate, craniosynostosis, submucous cleft palate, 22q11.2 deletion syndrome, Treacher Collins Syndrome, and CHARGE syndrome are just naming a few. I find I am very much involved with my children with a cleft palate, as I perform a standard 18-month evaluation post-palate repair to assess their current speech and language function. I also work closely with our surgeons and ENT team as the child grows to monitor for potential signs of velopharyngeal insufficiency, and participate in the nasopharyngoscopy procedures with our patients.
Does a child with a cleft palate have different speech characteristics than the children I see with phonological processes, and so forth?
YES! Although, keep in mind that a child with cleft palate can have a combination of both too! A reminder that many cases are not clear-cut and cannot fit into a perfect box or category. But often, these children have very unique speech errors that are specific to cleft palate, and these errors can persist even AFTER the cleft palate is repaired. Regular assessment and treatment methods with this population may not always work (although I love to come up with a unique treatment plan for each child).
If you have a child on your caseload with cleft palate, you should become acquainted with the proper evaluation tools and also be able to recognize/identify specific compensatory errors: glottal stops, coarticulations, nasal fricatives, pharyngeal fricatives, mid-dorsum palatal stops, backing, etc. If these are novel terms for you, I recommend checking out the continuing education resource recommendations below before moving forward. I think this will also help you feel more confident in your practice during evaluations and therapy sessions!

Okay, I’ve become acquainted with compensatory articulation errors and have identified them during my evaluation. I am ready to start treating. Where can I begin?
I love speaking about a child’s strengths when initially developing their treatment plan, in order to help use these sounds to facilitate our targets. Generally speaking, children with cleft palate have strengths in producing low-pressure sounds. These are sounds that do not require significant intraoral pressure in the mouth or are nasal sounds: /m, n, w, h, ng, l, r/. We often use these sounds and their placement cues to help the child learn a novel high-pressure sound—for example, utilization of strategy MMMMM –> B. The oral placement is the same, and the only thing that changes here is the manner. There are a number of different techniques you can learn on the LEADERSProject video modules, such as the one above, to help you facilitate the correct sound!
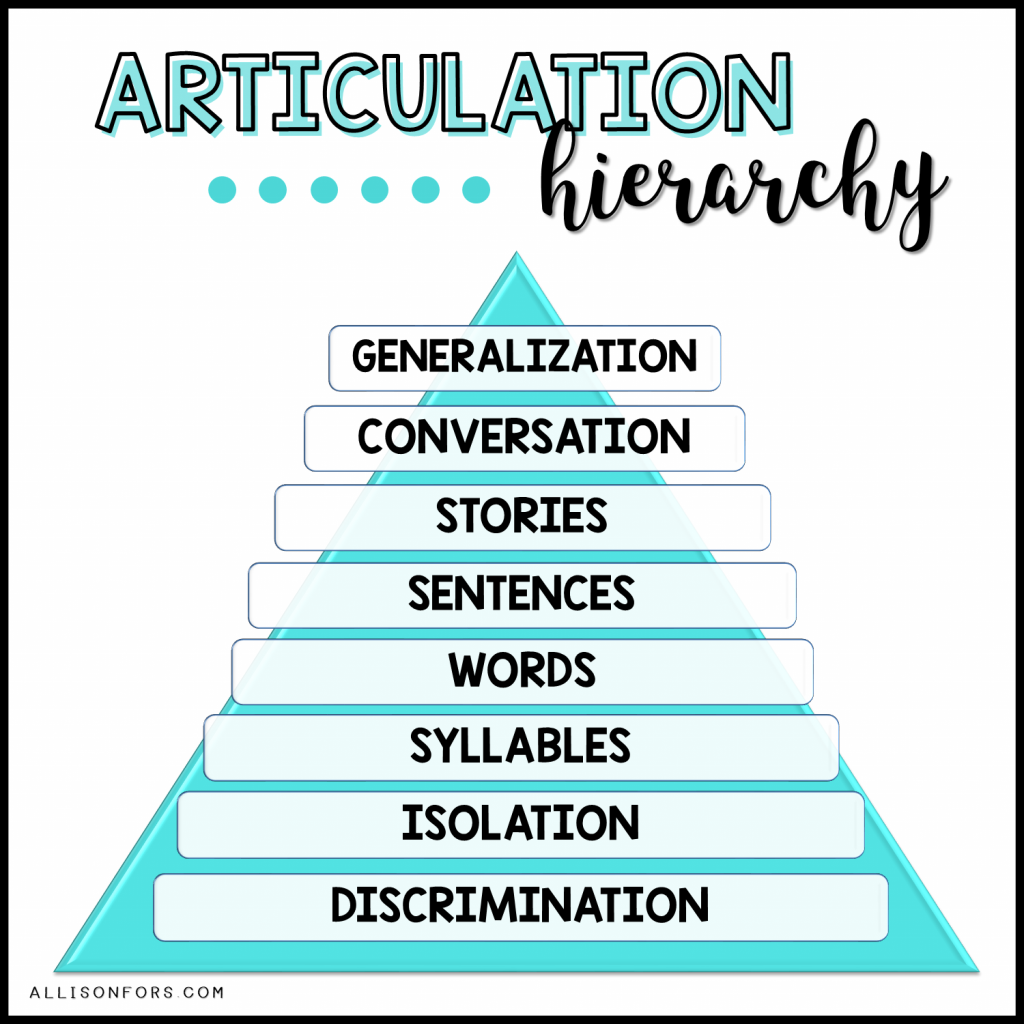
For cleft palate, I recommend taking a traditional hierarchy approach to help the child build up the necessary intraoral pressure for these sounds.
DISCRIMINATION: A key step, especially for our little ones! How can we expect them to make the correct sound if they don’t understand the difference? Instead of “correct” and “incorrect” differentiation, I like to use the terms “front” vs. “back” sounds, and “nose” vs. “throat” vs. “mouth” sounds.
SOUND IN ISOLATION
SOUND IN SYLLABLES
SOUND IN WORDS: Important to note that specifically for cleft palate, the target words should initially only include other low-pressure phonemes- so for example, if targeting /s/, “same” or “seen” or “less” would be a much better starting point than “stake” or “soup” where other high-pressure sounds are present. Like in regular therapy, I try to start out with monosyllabic targets and then increase syllable length from there. You can begin to incorporate words with other high-pressure sounds that the child has not yet achieved once he/she has mastered the initial word set.
SOUNDS IN PHRASES/SENTENCES: I love coming up with fun tongue twisters for this one, and even utilizing “functional home phrases” that can be targeted through the day! For /s/, we might utilize the terms “sit in your seat”, “so silly!”, or “I see ______” on a nature walk).
GENERALIZATION IN CONVERSATION: This is a crucial step, and in my opinion the hardest step, and often the one that SLPs forget about the most. I often walk my children around the clinic and have them engage in conversations with other adults/clinicians. You can ask the parents to set aside 30-60 min each day (sometimes at the dinner table) where they are monitoring the child’s target sound productions in a conversation, and then discuss the progress afterward. I have also implemented sticker charts in the classroom so that if a teacher, paraprofessional, or push-in SLP observes the child trying to make the target “mouth” sounds, then they can receive extra playtime or a prize after. It requires a lot of coordination across all environments to get this done, but I promise you it will set the child up for success and allow him/her to maintain these skills moving forward!
It is important to note that nonspeech oral motor exercises have not been shown in the research to help progress a child’s speech sound production within this population. While I use tactile cues during productions of the target sound to help facilitate correct placement, I never have the child engage in any blowing, sucking, tongue pulling, or stretching exercises.
How do I write my goals?
Okay, so, let’s say that our long term goal for our patient is to eliminate his coarticulations. An example of a SMART short term goal I would write might look like:
“XX will produce /p/ in the initial position of monosyllabic words using appropriate intraoral pressure with 85% accuracy across three sessions.”
Mentioning the oral airflow/intraoral pressure is important. As we know, he/she is currently trapping the airflow at the level of the glottis despite having good labial approximation. If you want to be more general with your goals, as I know from my school speechie friends that this is sometimes needed for IEPs, you could write:
“XX will produce bilabial stops /p, b/ using appropriate intraoral pressure at the sentence level with 85% accuracy across a semester.”
But for this goal, remember to still stick with the strict hierarchy mentioned above, and only go through the hierarchy with one sound at a time!
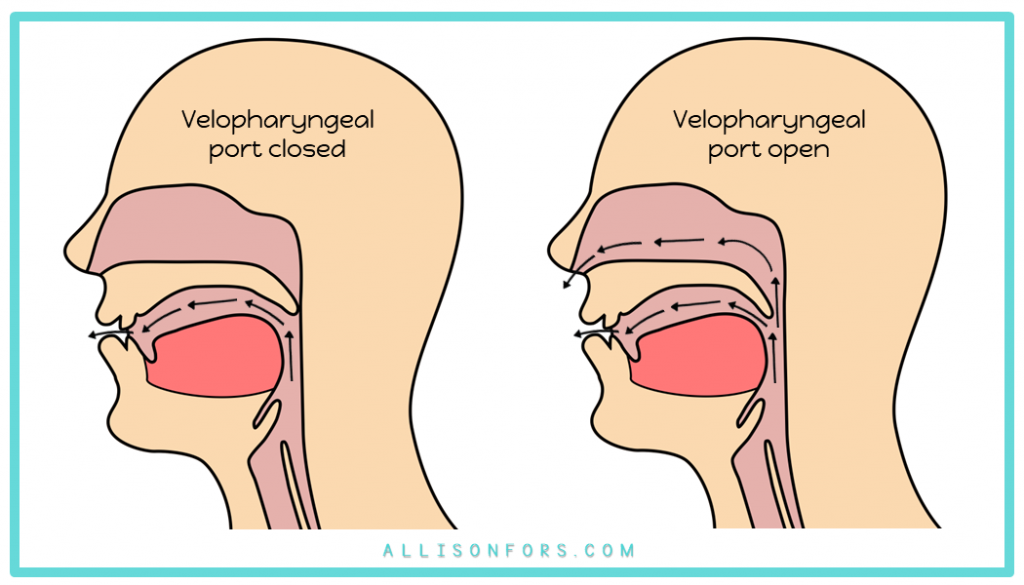
We have worked hard in therapy, but my child still has air escaping through the nose across all sounds despite having the tongue/lips in the correct place in the mouth. What do I do?
It is possible that your patient may have something known as velopharyngeal insufficiency. This is characterized by nasal air escape across all high-pressure sounds. (Important note: if nasal air escape is only present on one or two sounds, we know that this is phoneme-specific, and something that can be targeted in therapy/is not structural). Imaging, such as a nasopharyngoscopy or videofluoroscopy, is needed to confirm presence of VPI. If you think this may be the case for your child, reach out to the team craniofacial SLP and let them know about your clinical insight. Then the team can determine the next steps for assessment and imaging.
Where can I learn more?
- Feel free to follow me and send direct messages with questions at @thecraniofacialslp on Instagram! I post weekly tips and tricks for evaluation and therapy.
- Check out the ASHA Practice Portal on this Clinical Topic, available here: https://www.asha.org/Practice-Portal/Clinical-Topics/Cleft-Lip-and-Palate/
- LEADERSProject.org has some incredible, free, and easily accessible materials created specifically for children with cleft palate. Not to mention, the materials are produced in a number of different languages for easy family carryover!
- LEADERSProject also has AMAZING video modules available for *free* on Youtube that can advance your continuing education in this field, available here: https://www.youtube.com/watch?v=Lfoe9YiWkic and is a great place to start learning about the different compensatory errors mentioned in my blog post.
- I recommend attending talks about cleft lip/palate at the American Speech and Hearing Association Conference. And if you are really interested, attending the American Cleft Palate-Craniofacial Association (ACPA) Annual Meeting!
- The Clinician’s Guide to Treating Cleft Palate Speech by Peterson-Falzone, Trost-Cardamone, Karnell, and Hardin-Jones (2nd ed.) This book is a relatively affordable textbook that gives you a much more comprehensive look into what we do as SLPs on a Craniofacial Team, and how you too can become more confident with treating this population. I found this book helpful during my initial studies as it dives into a number of different clinical topics!
Are you interested in being a guest blogger? Fill out this form!





2 Responses
Hi,
I’ve been a Speech-Language Pathologist for over 20 years and I have my first prek student with cleft palate. I don’t know how to thank you for this information and resources. You’re amazing!
Sincerely,
Opal Heyward, SLP
I’m so glad! It’s definitely a niche area.