How to Help a Child with Sensory Processing Disorder Succeed in Speech Therapy
As SLPs, comprehending the sensory needs of children with sensory processing disorder allows us to better understand, help, and have more effective speech therapy sessions.
It is not uncommon for a child with sensory processing disorder (SPD) to also receive speech services. SPD is especially common in those diagnosed with autism – research shows 78% of autistic children present with sensory difficulties! [1] Often times children with SPD are viewed as lazy or as having behavioral issues when in reality the sensory problems are the cause. This is why it is crucial that, as SLPs, we gain an understanding of SPD and how to help a child with their sensory needs. In doing so, we can understand the root of the behavior, avoid meltdowns, and make progress in intervention.
What is sensory processing disorder?
Sensory processing disorder is when the brain has difficulty receiving, understanding, and responding to information that comes in via the senses. Children with SPD do not have adequate sensory processing skills to receive, organize, interpret and respond to sensory information efficiently. This negatively affects their attention, behavior, and development.
Indicators that a child may have sensory processing disorder:
- Unusually high activity level
- Unusually low activity level
- Displays poor body awareness – clumsy, difficulty with balance and motor skills, bumps into things
- Unpredictable and/or unsafe behaviors
- Behavior issues – short attention span, impulsivity, excessive tantrums
- Takes a long time to learn a new skill
- Display low muscle tone – floppy, leans on others for support
- Difficulty with academic areas despite normal intelligence
- Difficulty with gross and fine motor skills – handwriting, using scissors, tying shoes, buttoning, etc.
- Walks on toes
- Avoids certain textures while eating or playing, picky eater
- Chews on objects
- Struggles to focus and is easily distracted
- Over reacts to loud noises and dislikes crowded places
- Sensitive to certain clothing items
You may know that a child on your caseload has SPD because they have a diagnosis and are seeing an occupational therapist (OT). If you suspect a child has SPD, recommend them for an OT evaluation.
*Speech-language pathologists do not diagnose or treat SPD.
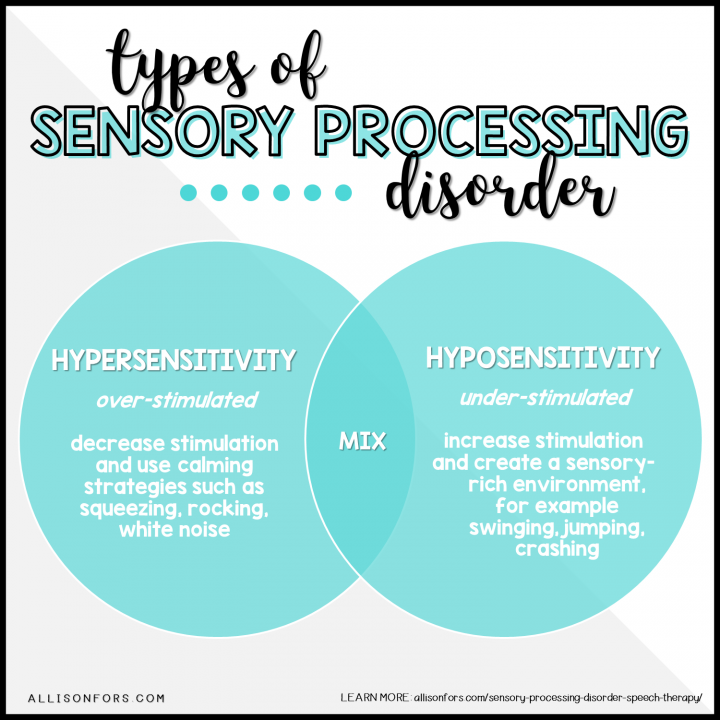
What are the different types of SPD? [2]
The symptoms of SPD are a spectrum and many children have a “mix” between being hypersensitive and hyposensitive.
HYPERSENSITIVE OR OVER-RESPONSIVE
Little stimulation overloads the sensory system. High-alert. May run away, lash out, scream, or hide and takes a long time to calm down after becoming upset.
- Hyper-Responsive Type: high level of arousal, distracted (eye darting and fidgety), irritable, impulsive.
- Avoidant Type: high level of arousal, fearful, anxious, avoids engagement and stimulation
HYPOSENSITIVE OR UNDER-RESPONSIVE
Requires a lot of stimulation to register sensory information. Lethargic. May seem tired, clumsy, or disinterested in activities.
- Hypo-Responsive Type: low level of arousal, lack of interest, passive engagement
- Sensory-Seeking Type: low level of arousal, sensory craver, seeks excessive movements, takes risks, want to touch everything, may seem to never get dizzy while spinning
What can we do in our sessions?
First off, if the child isn’t being seen by an occupational therapist, talk to the parents or the school OT about the OT services. If the student is seeing an OT, talk with them to get their suggestions on how to help that particular student with their sensory needs.
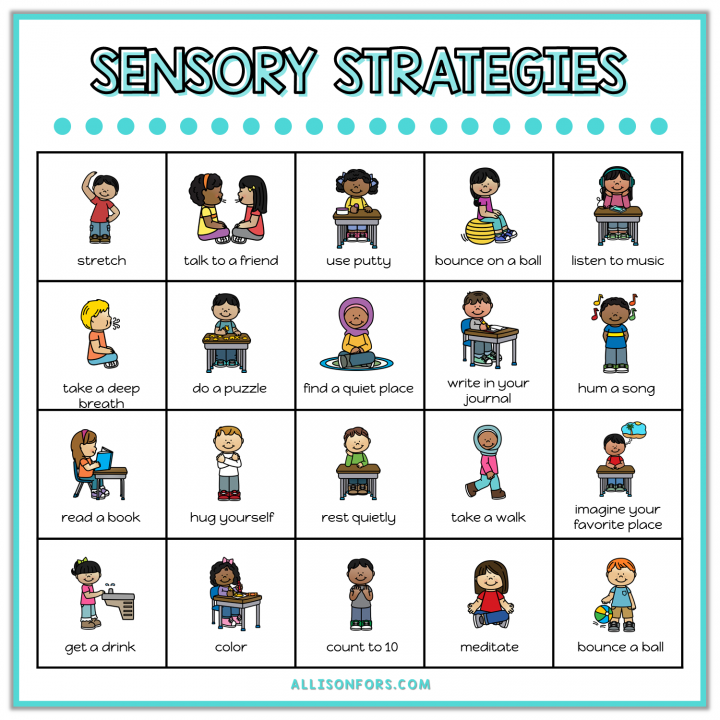
If the child is older and aware of their sensory difficulties, encourage them to communicate when they are feeling overwhelmed or underwhelmed. Discuss their sensory strategies with them and help him or her with them.
OVER-RESPONSIVE TYPES
Overall, try to decrease sensory experiences. A quiet, dim, enclosed space is ideal. If the child starts to get over-stimulated, use calming sensory strategies such as firm squeezes, rocking, white noise, and weighted blankets or vests. Avoid any toys or games with unexpected movements, loud sounds, or that are scented (markers, play dough). Using a visual schedule can help them anticipate future sensory experiences.
UNDER-RESPONSIVE TYPES
Overall, try to increase sensory experiences. Create a sensory-rich environment for the child to explore and engage with. Use alerting sensory strategies to help the child engage. For example, jumping, swinging, tickling, loud noises, crashing on a pad, and using sensory bins can help with the child’s attention. Try using novel and motivating toys and activities to increase engagement and sensory reactivity. The use of a visual schedule is also helpful.
Download the graphics found in this post for FREE!
Sensory Processing Disorder Myths
- “It’s a self-control issue” – The brain can have an overactive fight or flight response when it is struggling to interpret sensory information. This may present itself with self-control issues, but really the underlying issue is the brain’s ability to process the sensory information it is receiving.
- “They need to be disciplined” – Discipline and boundaries are important with any child but disciplining a child does not help them to process sensory information. It is more effective to help them understand why they are struggling, use sensory supports and visuals, and behavior strategies.
- “They are overreacting” – Children with SPD have a lower threshold for sensory input. Therefore they react more with tantrums, meltdowns, or acting out than their peers. They are not trying to be “naughty” or behavioral.
- “It is only about their senses” – SPD is more about the brain compared to senses. The brain process sensory and motor information and this is where the issue is resulting. This includes the five senses, as well as proprioception, interoception, and vestibular senses.
Websites for more information regarding SPD:
http://www.sensory-processing-disorder.com/
https://www.spdstar.org/basic/about-spd
[1] Miller, L.J., S. Schoen, J.Coll, B. Brett-Green, and M. Reale. Final report: Quantitative psychophysiologic evaluation of Sensory Processing in children with autistic spectrum disorders. Los Angeles, CA: Cure Autism Now, February 2005.
[2] Miller, L.J., Nielsen, D.M., Schoen, S.A. (2012). Attention deficit hyperactivity disorder and sensory modulation disorder: A comparison of behavior and physiology. Research in Developmental Disabilities, 33(3), 804-818.
If you enjoyed this post, please share it!
Follow my blog with Bloglovin






One Response
It’s interesting to learn that it’s not uncommon for a child with SPD to receive speech services. My wife and I are thinking that our son might have SPD and we were wondering how we can help him succeed in school. I’ll be sure to tell her that we should consider hiring speech services for our son.